Aorta
Aorta
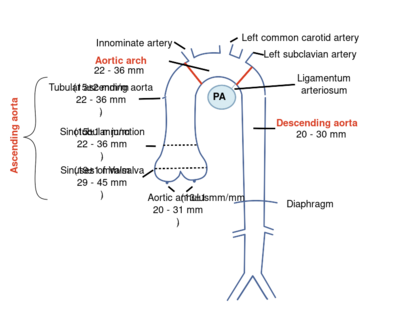
The thoracic aorta can be subdivided ito the aortic root (including the aortic annulus, aortic valve, and sinuses of Valsalva), the ascending aorta, the aortic arch, and the descending aorta.
|
| Picture source: Eur J Echocardiogr 2010;11:645-58[1] |
|---|
Aortic Dimensions
Aortic dimensions decrease from sinuses of Valsalva to the descending aorta.
| Aortic diameters (BSAindex) | |
|---|---|
| Aortic annulus | 20 - 31mm (13 ± 1mm/m2) |
| Aortic Root | 29 - 45 mm (19 ± 1 mm/m2) |
| Sinotubular junction | 22 - 36 mm (15 ± 1 mm/m2) |
| Tube | 22 - 36 mm (15 ± 2 mm/m2) |
| Aortic Arch | 22 - 36 mm |
| Descending aorta | 20 - 30 mm |
| Abdominal aorta | 20 - 30 mm |
| According to current recommendations measurements should be made using the leading edge to leading edge method, where callipers are placed on the outer layer of the anterior wall and the inner layer of the posterior wall. | |
Aortic dissection
Diagnostic is an undulating motion intimal flap, which in more recordings and directions must be seen. The flap should have a movement that is not parallel with any other cardio-thoracic structure.
| Upon dissection watch: |
|
|---|
It also shows the intramural hematoma of the aorta to be aware of the aortic dissection. One variant This does not intraluminal flap was observed making the diagnosis is difficult to establish. Echocardiographic is viewed as a thickened aortic wall.
| Differentiation between true and false lumen: |
|
|---|
Aortic coarctation
Imaging of the aortic arch usually works best from the jugular (sternal supra). When evaluating a patient with a suspected coarctation always pay attention to associated anomalies such as:
- Bicuspid aortic valve
- Aortic valve stenosis
- Patent ductus arteriosus
- VSD
- Mitral valve abnormalities
Determining coarctation[2]
| Instrument | Remark | |
|---|---|---|
| Location | Color doppler | The origin of the carotid and subclavian artery are reference points for locating the coarctation. |
| Speed Profile | Continuous wave | Remember that collaterals systolic maximum speed but does reduce the diastolic gradient persists. In the presence of diastolic forward flow refers to a hemodynamically significant coarctation.
Typical CW Doppler signal from descending aorta with diastolic forward flow matching hemodynamically significant coarctation. |
References
- Evangelista A, Flachskampf FA, Erbel R, Antonini-Canterin F, Vlachopoulos C, Rocchi G, Sicari R, Nihoyannopoulos P, Zamorano J, European Association of Echocardiography, Document Reviewers:, Pepi M, Breithardt OA, and Plonska-Gosciniak E. Echocardiography in aortic diseases: EAE recommendations for clinical practice. Eur J Echocardiogr. 2010 Sep;11(8):645-58. DOI:10.1093/ejechocard/jeq056 |