Mitral Insufficiency
Quantification mitral regurgitation[1]
| Slight | Moderate | Severe | |
|---|---|---|---|
| Jet plane surface/LA | <20% | 20-40% | >40% |
| Jet plane surface | <4cm2 | 4cm-10cm2 | 10cm2</sup |
| ERO | <20 mm2 | 20-40mm2 | 40mm2</sup |
| Vena contracta | <3mm | 3-7mm | >7mm |
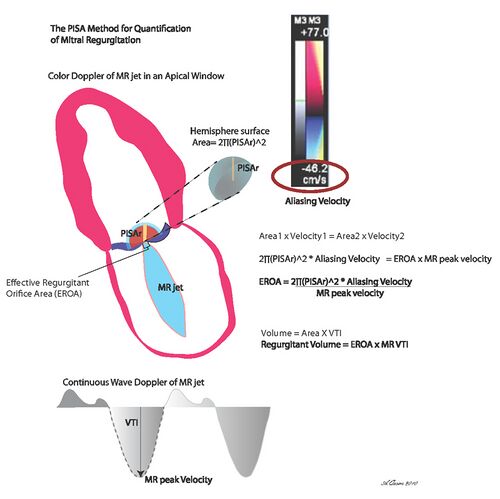
Click here for quantification mitral valvular insufficiency by PISA.
Assess the severity of mitral insufficiency
An independent measure seem to be that the regurgitant area trying to access parameters. With the help of the Proximal Isovelocity Surface Area (PISA) method, the effective regurgiterend orificium (ERO) can be calculated. The vena contracta (narrowest part of regurgitant jet) has a strong relationship with the regurgitant orificium.
Of course, it should not be forgotten. "Old" values in the estimation of the seriousness of the MI In a severe MI will, after all, often the left atrium will be enlarged and the PW measured with E / A ratio of the mitraalinflow >>1 should be, and the velocity E> 1.5 to 1.8 m/s.
| ||
|---|---|---|
| Criteria For MR severity* | ||
| Criteria | Mild MR | Severe MR |
| Regurgitant Volume | < 30 cc | > 60 cc |
| Regurgitant Fraction | < 30 % | > 50 % |
| EROA | < 0.20 cm^2 | > 0.40 mm^2 |
| *Moderate MR has values considered in between those of mild and severe both.[2] | ||
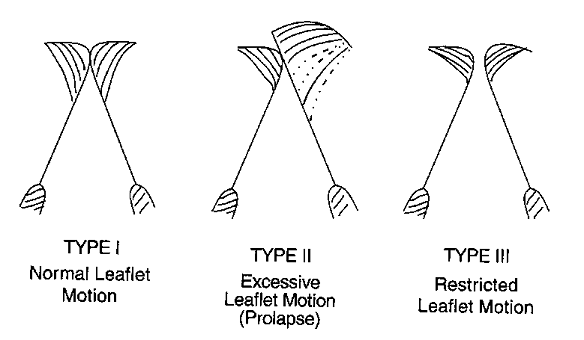
Carpentier classification
In the assessment of mitral regurgitation is important also the mechanism of mitral regurgitation study. Carpentier classified the mechanism of regurgitation into three groups:
Patients with mitral valve does not close completely, but which in diastole normal motility is seen are not easy to classify. This occurs in a highly dilated left ventricle or on the basis of myocardial ischemia. Carpentier shared this group with normal motility.
In addition to assessing the mobility of the mitral valve apparatus must also be paid to the apposition of the mitral valve coaptation and magazines. Coaptation is the contact area of both leaflets when the valve is closed. Apposition, the valve blades in contact with each other (symmetrical or asymmetrical).
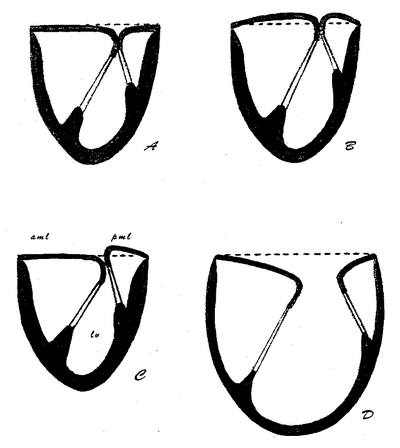
|
|
A: Normal coaptation and apposition B: Billowing allowing coaptation point moves towards the bosom, normal apposition C: Reduced zone of coaptation by abnormal apposition D: Total loss of coaptation with normal apposition[3] |
References
- Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, Hagendorff A, Monin JL, Badano L, Zamorano JL, and European Association of Echocardiography. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010 May;11(4):307-32. DOI:10.1093/ejechocard/jeq031 |
- de Marchena E, Badiye A, Robalino G, Junttila J, Atapattu S, Nakamura M, De Canniere D, and Salerno T. Respective prevalence of the different carpentier classes of mitral regurgitation: a stepping stone for future therapeutic research and development. J Card Surg. 2011 Jul;26(4):385-92. DOI:10.1111/j.1540-8191.2011.01274.x |