Pulmonary Hypertension: Difference between revisions
Jump to navigation
Jump to search
(Created page with "Pulmonary hypertension is a rare cause of high blood pressure ( hypertension ) in the pulmonary artery ( pulmonary artery ) . When the blood vessels of the lungs may be damage...") |
No edit summary |
||
| (15 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__TOC__ | |||
Pulmonary hypertension is a rare cause of high blood pressure (hypertension) in the pulmonary artery (pulmonary artery). When the blood vessels of the lungs becomes damaged, such as in pulmonary arterial hypertension, the thickening and stiffening of the pulmonary artery walls occur which causes deviations in the vessel wall. The consequence of this is that the pressure in the pulmonary artery rises and also in the RV. PH is a pressure load on the right heart. Click [http://www.youtube.com/watch?v=ROz1XSWwxR4 '''here'''] to see an animation about PH. | |||
Pulmonary hypertension is | |||
classification | ==WHO classification== | ||
Pulmonary | Pulmonary hypertension is classified by the World Health Organization (WHO) as the place where the obstruction lies. | ||
{| class="wikitable" cellpadding="0" cellspacing="0" border="0" width="800px" | |||
|- | |||
!Classification | |||
!Subcategories | |||
|- | |||
!valign="top"|Pulmonary Arterial Hypertension(PAH) | |||
| | |||
*Idiopathic PAH(unknown cause) | |||
*Familial PAH(genetic cause) | |||
*PAH by underlying causes such as, connective tissue diseases, congenital heart disease, portal hypertension, HIV infection, drugs, drugs, toxins, and other factors. | |||
*PAH with significant venous and/or capillary involvement | |||
*Persistent pulmonary hypertension of newborn | |||
|- | |||
!valign="top"|Pulmonary hypertension with left heart disease | |||
| | |||
*In disorders of left atrium and ventricle of the heart | |||
*With Valvular | |||
|- | |||
!valign="top"|Pulmonary hypertension in pulmonary disease and/or hypoxemia | |||
| | |||
*Chronic obstructive pulmonary disease(COPD) | |||
*Interstitial lung disease | |||
*Sleep disorders, alveolar hypoventilation; chronic exposure to high altitude | |||
Pulmonary hypertension | *Congenital malformations/developmental | ||
|- | |||
!valign="top"|Pulmonary hypertension due to chronic thrombotic and/or embolic processes | |||
| | |||
*Thromboembolic obstruction of proximal pulmonary arteries | |||
*Thromboembolic obstruction of distal pulmonary arteries | |||
*Embolism of the lung (eg: tumor, parasites, foreign body, bone marrow) | |||
|- | |||
!valign="top"|Pulmonary hypertension as a result of other diseases and disorders | |||
| | |||
*Sarcoidosis | |||
*Histiocytosis X | |||
*Lymphangioleiomyomatosis | |||
*Sickle Cells | |||
*Compression of the pulmonary vessels from outside(eg: by lymphadenopathy, tumor, fibrosing mediastinitis) | |||
*Storage disorders | |||
of | |} | ||
==Evidence of pulmonary hypertension== | |||
{| class="wikitable" cellpadding="0" cellspacing="0" border="0" width="800px" | |||
|- | |||
! | |||
!Unlikely | |||
!Possible | |||
!Likely | |||
|- | |||
!SPAP | |||
|align="center"|<36 mmHg | |||
|align="center"|36-50 mmHg | |||
|align="center"|>50 mmHg | |||
|- | |||
!TR Vmax | |||
|align="center"|<2.8 m/s | |||
|align="center"|2.9-3.4 m/s | |||
|align="center"|>3.4 m/s | |||
|- | |||
!AccT | |||
|align="center"|>120 ms | |||
|align="center"|120-60 ms | |||
|align="center"|<60 ms | |||
|- | |||
!RV MPI (TCO-ET/ET) | |||
|align="center"|<0.36 | |||
| | |||
| | |||
|- | |||
!RV MPI (TDI) | |||
|align="center"|<0:50 | |||
| | |||
| | |||
|} | |||
==Calculations for estimating pressure in the pulmonary artery== | |||
{| class="wikitable" cellpadding="0" cellspacing="0" border="0" width="800px" | |||
|- | |||
! | |||
!Formula | |||
|- | |||
!Systolic PA pressure | |||
|4 x(TR Vmax)<sup>2</sup> + estimated RA pressure | |||
|- | |||
!Diastolic PA pressure | |||
|4 x(PR Ved)<sup>2</sup> + estimated RA pressure | |||
|- | |||
!rowspan="4" valign="top"|Mean PA pressure | |||
|0.3 x systolic PA pressure + 0.6 x diastolic PA pressure | |||
|- | |||
|90 - (0.62 x ACCT) if Acct < 120ms | |||
|- | |||
|4 x(PR Vmax)<sup>2</sup> + estimated RA pressure | |||
|- | |||
|TR PGmean + estimated RA pressure | |||
|} | |||
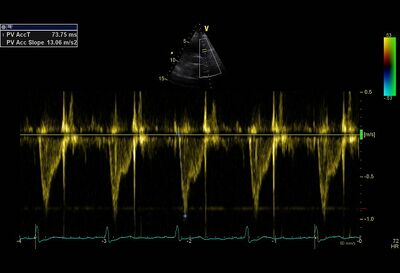
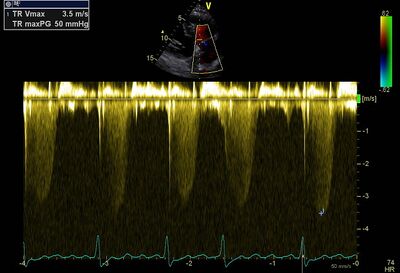
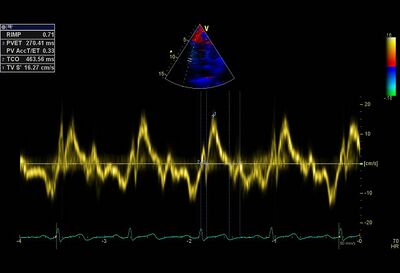
==Examples of severe pulmonary hypertension<cite>1</cite>== | |||
Short | {| class="wikitable" cellpadding="0" cellspacing="0" border="0" | ||
|- | |||
|[[Image:PVAccT02.jpg|400px]] | |||
|Video | |||
|- | |||
!Short AccT with "systolic notch" | |||
!Flattened septum | |||
|- | |||
|[[Image:SPAP01.jpg|400px]] | |||
|[[Image:PAH01.jpg|400px]] | |||
|- | |||
!Increased Systolic PA pressure | |||
!Increased MPI, extension of isovolumetric times | |||
|} | |||
==References== | |||
<biblio> | |||
#1 pmid=22941889 | |||
</biblio> | |||
Latest revision as of 21:55, 7 February 2014
Pulmonary hypertension is a rare cause of high blood pressure (hypertension) in the pulmonary artery (pulmonary artery). When the blood vessels of the lungs becomes damaged, such as in pulmonary arterial hypertension, the thickening and stiffening of the pulmonary artery walls occur which causes deviations in the vessel wall. The consequence of this is that the pressure in the pulmonary artery rises and also in the RV. PH is a pressure load on the right heart. Click here to see an animation about PH.
WHO classification
Pulmonary hypertension is classified by the World Health Organization (WHO) as the place where the obstruction lies.
| Classification | Subcategories |
|---|---|
| Pulmonary Arterial Hypertension(PAH) |
|
| Pulmonary hypertension with left heart disease |
|
| Pulmonary hypertension in pulmonary disease and/or hypoxemia |
|
| Pulmonary hypertension due to chronic thrombotic and/or embolic processes |
|
| Pulmonary hypertension as a result of other diseases and disorders |
|
Evidence of pulmonary hypertension
| Unlikely | Possible | Likely | |
|---|---|---|---|
| SPAP | <36 mmHg | 36-50 mmHg | >50 mmHg |
| TR Vmax | <2.8 m/s | 2.9-3.4 m/s | >3.4 m/s |
| AccT | >120 ms | 120-60 ms | <60 ms |
| RV MPI (TCO-ET/ET) | <0.36 | ||
| RV MPI (TDI) | <0:50 |
Calculations for estimating pressure in the pulmonary artery
| Formula | |
|---|---|
| Systolic PA pressure | 4 x(TR Vmax)2 + estimated RA pressure |
| Diastolic PA pressure | 4 x(PR Ved)2 + estimated RA pressure |
| Mean PA pressure | 0.3 x systolic PA pressure + 0.6 x diastolic PA pressure |
| 90 - (0.62 x ACCT) if Acct < 120ms | |
| 4 x(PR Vmax)2 + estimated RA pressure | |
| TR PGmean + estimated RA pressure |
Examples of severe pulmonary hypertension[1]
|
Video |
| Short AccT with "systolic notch" | Flattened septum |
|---|---|
|
|
| Increased Systolic PA pressure | Increased MPI, extension of isovolumetric times |