Pericarditis/Tamponade
Pericarditis is an inflammation of the pericardium (heart sac) usually caused by a virus. Echocardiographic is often seen in the pericardium (pericardial effusion). A fatal complication of pericarditis is that an inflammation in the heart causes the pericardial fluid or blood to fill up when relaxed, this is called tamponade.
| Video |
| Tamponade picture with large amount of pericardial |
|---|
Inflow obstruction
At pericarditis or tamponade, there is an obstacle for intake from the atria to the ventricles. Due to the obstruction from outside, eg by the pericardial fluid, the space in the heart becomes restricted and the filling of one ventricle becomes detrimental to the area of the other ventricle. When inhaling the filling of the right ventricle does at the expense of the filling of the left ventricle. This is called interdependence. During tamponade, the outside pressure causing this effect is much more to the ground compared with constrictive pericarditis when the early diastolic filling is not obstructed. This is also always why a tamponade throughout the diastolic filling is almost the reason Pulsus paradoxus is found only rarely in a constrictive.
Inhalation decreases the intrathoracic pressure and thus the pressure longveneuse will also decrease, however the intrapericardially situated diastolic LV pressure will not fall. In other words, by inhalation, reduction in the pressure gradient between the pulmonary veins and left ventricle which result in the filling up of the left ventricle.
|
|---|
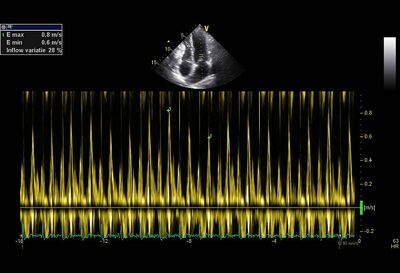
| MV inflow variation >25% |
| Echocardiographic findings at a major inflow obstruction | |
|---|---|
| Doppler |
|
| 2 - D images |
|
| However, early after cardiac surgery, there may be geloketteerd pericardial. This may cause local compression to occur, and the evidence of inflow obstruction more difficult to interpret. | |
Doppler measurements
Evidence of an inflow impediment to the LV and RV expressing itself in elevated filling pressures. The mitral and tricuspid inflow pattern will play an E/A ratio >1 exhibit generally. Also, the deceleration time will be of the mitral E- top shortened (<180 msec.) In the pulmonary vein flow, the S- wave will be smaller than the D- wave.
In a constrictive the right and left ventricular filling influence each other. The following indications point to this:
- Respiratory variation in MV inflow (at start of inspiration decline MV inflow E -top >25%) and TV inflow (at start of inspiration increase of E -top >40%).
- Respiratory variation in pulmonary vein flow wherein at the beginning of expiration the diastolic forward flow >10% increase.
Also, atrial fibrillation, this respiratory variation can be observed. In severe obstructive pulmonary same pattern can be seen. Reinforced by the change in intrathoracic pressure However, this will also increase sharply to the right ventricle during inspiration caval flow. In a constrictive flow will hardly increase.
After a pericardiectomy often still an abnormal filling pattern is observed. On the one hand it is thought that this is due to incomplete pericardiectomy. On the other hand this is possible because the myocardium is sometimes involved in the disease process. The measured with TDI early diastolic velocity of the mitral valve annulus septal (E ') often taken postoperatively decreases, which would fit in a relaxation disorder of the myocardium. This may explain in autopsies the increased myocardial fibrosis that is found. The disease process which gave constriction, can also cause myocardial fibrosis (radiotherapy, auto- immune processes). The emergence of a more restrictive image after pericardiectomy is associated with a worse prognosis.
Constrictive pericarditis
Constrictive pericarditis is a form of pericarditis in which the pericardium is thickened and it were a hard shell that forms around the heart. This is also called "armored heart". Thus, the heart can not fill normally (diastolic dysfunction). Inhalation reduces the pressure in the chest. Due to the lower pressure more blood can flow to the right ventricle. This bends the ventricular septum to the LV far. The LV thus therefore becomes less filled.
| Evidence of constrictive pericarditis | |
| M -mode |
|
| 2 - D images |
|
It is necessary to realize that specific deviations do not suggest a constrictive pericarditis. Such deviations are observed in other syndromes also. It is the combination of different deviations that gives a strong indication of a constrictive pericarditis.
Constrictive pericarditis vs Restrictive cardiomyopathy
The image of a pericarditis resembles the image of a restrictive cardiomyopathy: good systolic LV function with diastolic dysfunction. However, there are differences that can be distinguished with echocardiography. In restrictive cardiomyopathy, there is a myocardial disease. Primarily, it is the function disorder of the myocardium. Therefore, often deviations with regards to myocardial are observed, for example like the speckled aspect, thickened valves, thickened atrial septal amyloidosis and also a reduced systolic function. Dysfunctions can also be detected even if it is not part of the constrictive pericarditis. At a restrictive cardiomyopathy the atria are often greatly enlarged with a restrictive cardiomyopathy. In a constrictive, there is also often some atria dilatation but this is not conspicuous. The mitral inflow patterns in a restrictive cardiomyopathy often shows a more pronounced restrictive filling pattern, E/A ratio of 2 or higher with deceleration times shorter than 140msec. In a restrictive cardiomyopathy, pulmonary hypertension can sometimes be a significant action (>50 mmHg). In a constrictive, there is rarely a pulmonary pressure above 50 mmHg found.
More specific effects are shown in the table below :
| Constriction | Restriction | |
|---|---|---|
| Septal motion | Respiratory shift | Normal |
| Mitral E/A ratio | >1.5 | >1.5 |
| Mitral DecT (ms) | <160 | <160 |
| Mitral inflow respiratory variation | Usually present | Absent |
| Hepatic vein Doppler | Expiratory diastolic flow reversal | Inspiratory diastolic flow reversal |
| Mitral septal É (cm/s) | >7 | <7 |
| Mitral lateral É | < septal É | >É septal |
| Ventricular septal strain | Normal | Reduced |
| Video |
References
- Rajagopalan N, Garcia MJ, Rodriguez L, Murray RD, Apperson-Hansen C, Stugaard M, Thomas JD, and Klein AL. Comparison of new Doppler echocardiographic methods to differentiate constrictive pericardial heart disease and restrictive cardiomyopathy. Am J Cardiol. 2001 Jan 1;87(1):86-94. DOI:10.1016/s0002-9149(00)01278-9 |